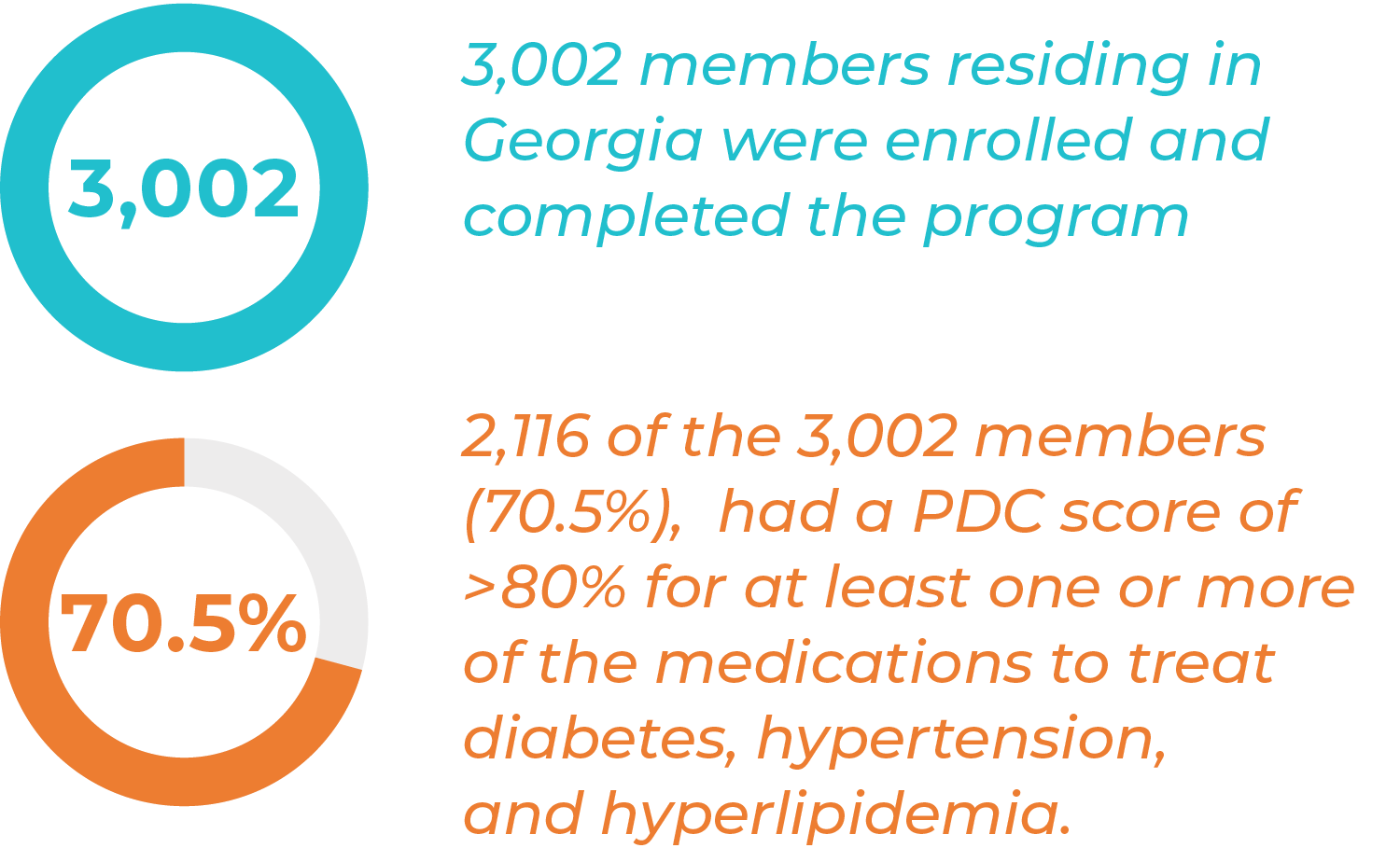
3,002 Members Residing in Georgia Were Enrolled and Completed the Program
C3 HealthcareRx focused on medication adherence in members with diabetes, hypertension and or hyperlipidemia.
Overview
C3’s Medication Management Adherence Measures Program was in partnership with a large health plan‘s Medicare and Retirement division. The program targeted members who had been identified non-compliant with their specific medications to treat diabetes, hypertension, and/or hyperlipidemia.
The goal was to target 3,000 members residing in Georgia. C3 certified pharmacy technicians (CPhTs) and Pharmacists supported members through a 10-month program to increase members’ adherence to their medication regimens. PDC (proportion of days covered) scores were used to measure members’ adherence. A PDC score of > 80% for each diabetic, antihypertensive, and/or antihyperlipidemic medication defined a member as compliant.
Health plan provided a list of members with PDC scores below 80% who were not responsive to internal efforts to increase adherence. The performance goal was to increase or maintain a PDC score of greater than 80% or higher for targeted population.
Solution
Program launched in February of 2020, where member lists and claims data were utilized to target population below 80% PDC.
Patient Care Coordinators (PCCs) enrolled members into the program and performed telephonic medication reconciliations and assessments to identify barriers to medication compliance.
All member assessments were reviewed by a C3 pharmacist and additional pharmacist counseling, education, or intervention was performed as necessary. PCCs engaged patients telephonically throughout the rest of the calendar year to conduct PDC calls 10 days prior to medication refills.
Key Outcomes
During the telephonic period, C3 had an acceptance rate of over 73% of patients reached into the program.
Download a PDF of this case study, here. For more information, please call (888) 411-1520.